In the days leading to his death, former Marine Cpl. Jason Simcakoski texted his dad from the inpatient psychiatric ward at the Tomah, Wisconsin, Veterans Affairs hospital.
"I slept horrible last night," Simcakoski wrote Aug. 27, 2014. "I tossed and turned sweating … then I just stayed up. I couldn't take it. I'm worse now than before I came in."
Simcakoski had checked himself in for chronic drug misuse, anxiety and post-traumatic stress disorder. He was taking 14 medications — including antipsychotics, muscle relaxers, antidepressants and tramadol, a powerful opioid painkiller prescribed to him by Tomah doctors.
In the psych ward, physicians added another drug, suboxone, to the mix. The medication is used to treat opioid addiction but is itself a combination of narcotics that can cause respiratory distress.
On Aug. 30, Simcakoski awoke complaining of a headache. He was given an analgesic to dull the pain and left to rest.
He never woke up. He died from an accidental overdose — "multiple drug toxicity," according to records.
"I assumed he would sleep and wake up and it would be fine," said his widow, Heather Simcakoski, who visited Jason that morning. "He was an inpatient. Never in a million years would I think he could die."

Jason Simcakoski
Photo Credit: Contributed
Jason Simcakoski is one of countless post-9/11 veterans since at least 2005 who have died by accidental overdose under VA care. The families of former Marine Sgt. Rob Richards, Senior Airman Anthony Mena, Marine Gunnery Sgt. Christopher Bachus, Marine Cpl. Nicholas Endicott, Marine Cpl. Andrew White and others share the inescapable memory of either finding their loved one deceased or receiving a devastating phone call.
A 2011 VA study based on 2005 data — the most recent public VA analysis — found that veterans ages 18-29 who received care at VA died of accidental overdoses at 1.5 times the rate of civilians their own age, Those ages 30-64 had overdose rates more than twice the civilian rate.
Since 2007, lawmakers have grappled with the problem, hearing testimony from family members with horror stories of drugged veterans and former troops with multiple prescriptions, taking narcotics or opioids and benzodiazepines with deadly results.
Lawmakers have tried to pass legislation to improve prescribing transparency at VA, increase access to care for substance abuse disorders and provide options at VA for pain management using other than narcotic painkillers. But most attempts have failed.
This week, Sen. Tammy Baldwin, D-Wis., will try again.
Smarting from reports that she failed to follow up on problems at the Tomah VA, as well as an investigation published in January by the Center for Investigative Reporting that said the facility was known as "Candy Land" among veterans for its painkiller dispensing habits, Baldwin will introduce legislation to strengthen VA's oversight of opiate drug prescriptions and pain management programs.
Baldwin's proposed Jason Simcakoski Memorial Opioid Safety bill would create a number of safeguards to protect veterans and improve VA medical care. It would require VA and the Defense Department to update clinical practice guidelines for opioid therapy for pain; mandate training for VA doctors who prescribe opioids; and create pain management boards in all VA regions that would oversee compliance of pain management practices at each VA facility.
Baldwin said the legislation is needed to give medical professionals greater guidance for treating veterans with physical pain and mental health conditions and empower patients and family members to manage their care.
"This is a response to the significant increase in addiction and over-reliance on opioids both within the VA and on the outside," she said.
The bill also would require VA to develop plans for researching and incorporating alternative pain management therapies into treatment. Many VA hospitals and clinics offer alternative therapies like acupuncture, biofeedback, yoga, meditation and art therapy for pain management and behavioral health, but programs are inconsistent across VA hospitals, Baldwin said.
"If you look at what's provided at facilities and the distances some veterans have to travel to get to facilities, access to complementary and alternative treatment is uneven across this country," she said. "We have a long way to go to figure out what works best."
At Tomah, it appears that painkillers often were the first line of treatment for any and all ailments.
According to the CIR report, the number of opiate prescriptions at the Tomah VA quintupled from 2004 to 2012, with rates rising sharply after the medical center hired Dr. David Houlihan, a psychiatrist, as chief of staff.
When pharmacists raised questions about the high number of prescriptions, they faced retaliation, were fired or resigned in protest.
A clinical psychologist who expressed concern about questionable practices at Tomah in 2009 died by suicide shortly after he was fired for blowing the whistle on patient medications.
At least six deaths at the facility have been tied to medications or considered suspicious at the facility.
A VA inspector general report also found that Houlihan prescribed the equivalent of 25,000 milligrams of morphine to each of the 128 patients he saw in 2012, a level the IG said "raised potentially serious concerns." That report was not made public until after the CIR investigation was published.
Baldwin said she asked VA Secretary Bob McDonald to investigate as soon as she learned about the "unspeakable tragedy" from media reports.
Simcakoski said she was heartbroken to find the problems were known well before her husband died.
"Never did I know any of this was a concern at the hospital. Jason chose the facility because he heard it had excellent mental health programs," Simcakoski said.
VA officials say they have implemented new measures to monitor opioid prescriptions at facilities, to include tracking them at the regional level and rolling out a system to monitor prescriptions at the doctor and patient level.
And, according to VA, since the department's Opioid Safety Initiative was introduced in 2013, the number of veterans prescribed opioids has dropped by nearly 110,000, and the number receiving opioids and benzodiazepines together — a mix that can cause respiratory distress and accidental death — declined by nearly 34,000.
Baldwin noted that progress but said she'd like the figures to drop further. She added, however, that her goal is not to take pain medications away from those in physical pain.
"What we've learned is that too many of our veterans are becoming hooked on opioids and they need the VA to help not get them hooked," Baldwin said.
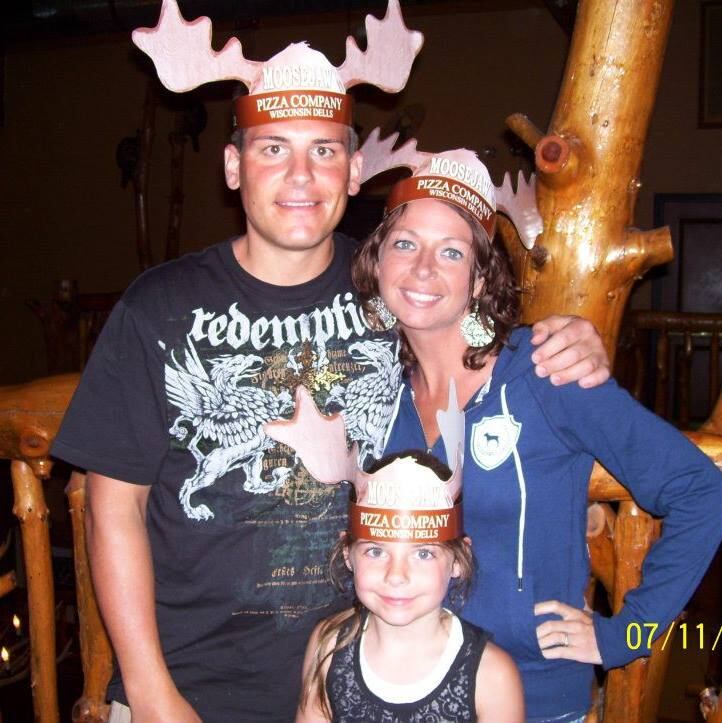
Heather Fluty Simcakoski, right, her husband Jason Simcakoski and their daughter Anaya Simcakoski.
Photo Credit: Courtesy of Heather Fluty Simcakoski
The week of June 22, Heather Simcakoski will travel with daughter Anaya to Washington, D.C., to support Baldwin as the senator introduces her bill.
She called it a "huge relief that people are finally listening."
"This is painful and it's never going to change what happened to Jason. But he always knew his life had meaning. I'm not sure he felt it at the end, but he was right. This brings meaning to Jason's life," Simcakoski said.
Patricia Kime is a senior writer covering military and veterans health care, medicine and personnel issues.





