Master Sgt. Geoff Dardia was nearly a decade into his Special Forces career when he says he hit a wall. He was struggling both mentally and physically to keep doing his job and couldn’t explain why.
“All of the sudden, I was just a shell of a person — like everything you hear about feeling like you’re dragging a dead body and losing your zest for life,” Dardia said.
Plagued by severe migraines, fatigue and issues with his balance and vision, Dardia, now 44, sought help.
His superiors told him to visit a military behavioral health specialist and be treated for PTSD or depression, but Dardia was convinced his ailments were more than just psychological. So, he did what any good Green Beret would do and applied his training to research, analyze and attack the problem condition.
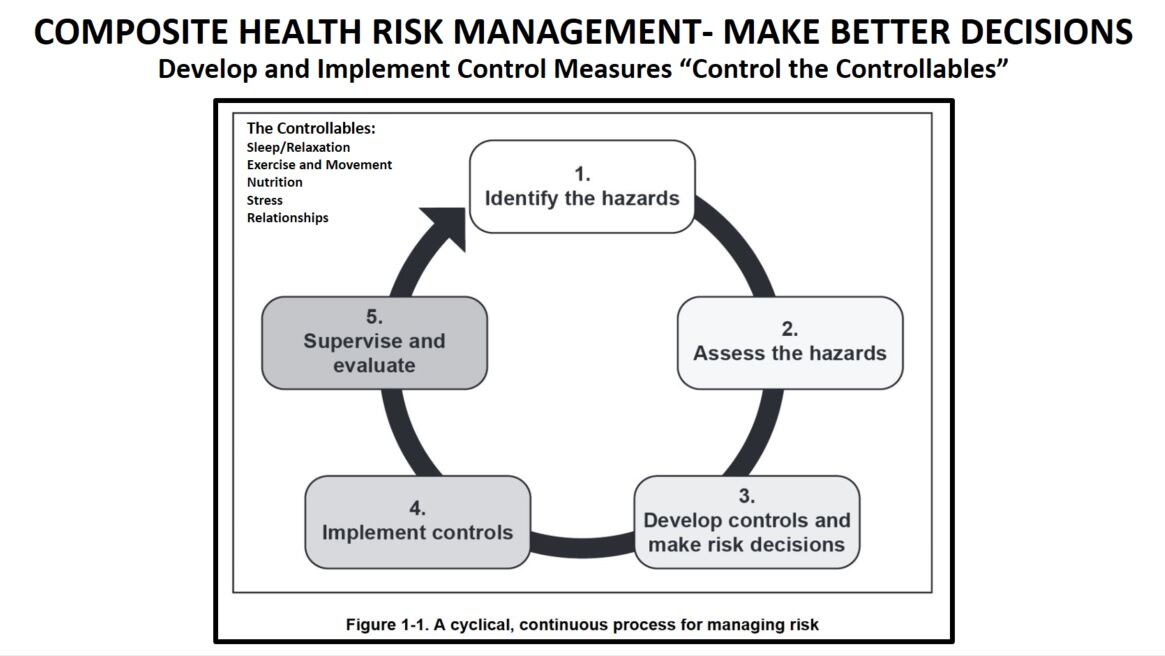
Following the steps of the military decision-making process, Dardia learned everything he could about his operational environment and the various ways it could affect him.
Traumatic brain injuries, toxic exposure to heavy metals and carcinogens, traumatic stress and sleep deprivation are unfortunately common occurrences for members of the special operations community.
After identifying the underlying causes for his symptoms, Dardia began planning a course of responsive action. The process was so simple, straightforward, and guided by existing military doctrine that it led him to question the Army’s current approach to health care.
“I was like, ‘This is so easy. Why wouldn’t we do this with health and wellness and medicine?’” Dardia said.
At its core, that’s what functional medicine is all about: finding and treating underlying causes of illness or pain. The Institute for Functional Medicine defines it as “a systems biology-based approach that focuses on identifying and addressing the root cause of disease.”
Also referred to as personalized, performance or lifestyle medicine, the approach is grounded in a philosophy of caring for a whole person made up of interconnected parts.
It’s what Dardia and health care professionals spoke about on March 25 at the Warfighter Health Symposium in Tampa, Florida. Hosted by non-profits Task Force Dagger Special Operations Foundation and HunterSeven, the event served to informally educate active duty servicemembers, medical providers and veterans about the current issues and solutions in military health care. There were 50 people — the maximum allowed under COVID-19 restrictions — who attended.
After personally experiencing the difficulty of receiving holistic treatment, Dardia began making the changes he wanted to see. In 2012, when TFDSOF helped him through his personal health struggles, Dardia decided to give back by founding the organization’s Health Initiative Program.
The program provides pathways and funding assistance for members of the military to seek treatment from outside health care providers and institutions in the field of personalized medicine.
Partnering with organizations like the Cleveland Clinic Center for Functional Medicine and becoming involved with active-duty health initiatives in the 3rd Special Forces Group, Dardia has been raising awareness of the power of preventative and holistic medicine for the better part of a decade now.
According to Dardia, the military’s current approach to health care is too reactive. Service members are treated for cancer or suicidal ideations or organ failures when such issues could have been prevented with proper countermeasures and education about their causes years earlier.
“Just because you have mental health symptoms, doesn’t mean mental illness is the cause,” said Dr. Carrie Elk, founder of the Elk Institute for Psychological Health & Performance, a non-profit established to provide mental health education and treatment to servicemembers.
Elk has worked with SOCOM and the SOF community to treat operators for the underlying cause of post-traumatic stress disorder since 2010, when she first spoke at the Joint Special Operations Forces Senior Enlisted Academy on how PTSD works. Her practice now reaches both operators and members of the general military community.
“They were applying the same stuff they used for mental illness to PTSD, but the problem is just the way the information is stored,” said Elk. The audience was stunned by Elk’s presentation, and special operations personnel began filling the waiting room of her practice.
In just two hours of therapy, the doctor says, she’s able to correct the storage of a traumatic memory.
In traumatic situations, according to Elk, memories are stored as sensory experiences. When servicemembers return home from traumatic environments, triggers like smells and sounds can bring them right back to places of anger, agitation, depression and anxiety.
Health care providers treating symptoms of depression and anxiety with prescription medications ignore the real problems at hand, according to Elk.
“We’re putting a Band-Aid on a bullet hole — or at least trying to,” said Elk. “You’re not fixing the cause, you’re just managing symptoms when you don’t have to.”
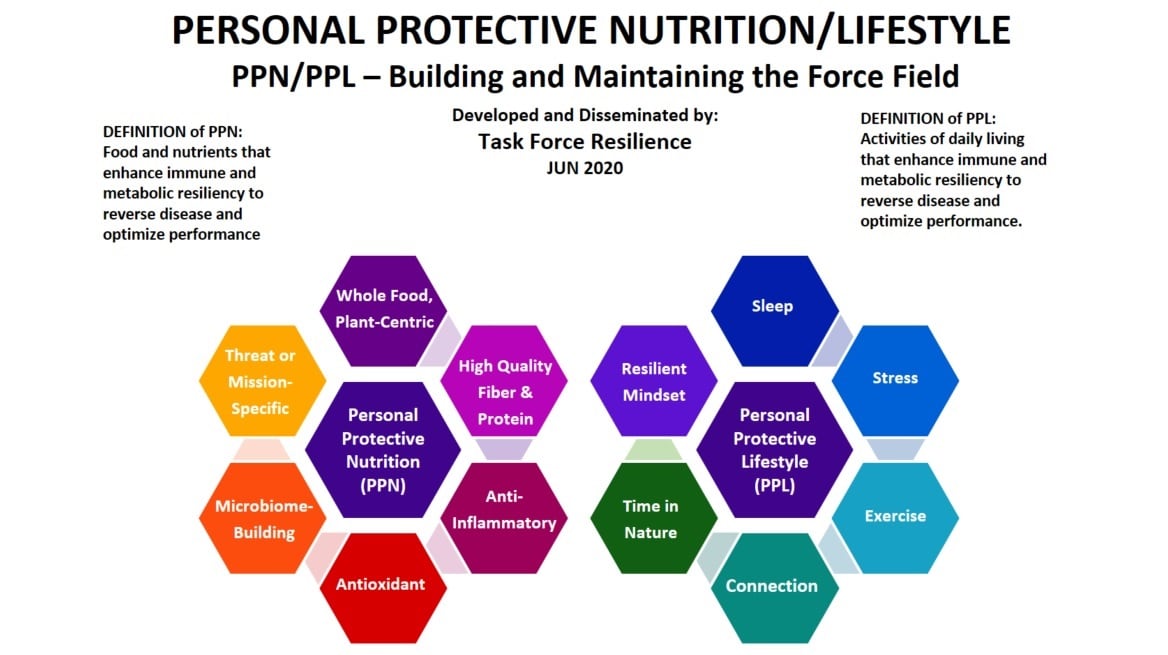
Functional approaches like Elk’s are growing in popularity. The Army adopted a section on holistic health in its updated physical fitness doctrine in September 2020 — a combination of its previous initiatives like the Performance Triad and Army Wellness Centers.
The Holistic Health and Fitness program, or H2F, “is the framework to encompass all aspects of human performance to include physical, sleep, nutritional, spiritual, and mental fitness,” said Maj. Gen. Lonnie G. Hibbard, commander of the U.S. Army Center for Initial Military Training in a press release.
The Department of Veterans Affairs has introduced similar programming aimed at addressing the causes of illness rather than symptoms.
“The biggest thing is awareness and education and advocacy,” said Dardia. The earlier servicemembers can learn to prevent toxic exposure and recover from stress and sleep deprivation, the healthier they’ll be in the long term.
Now the operations sergeant for 3SFG’s Human Performance and Wellness program and the Medical Education Transition Advocacy and Assistance program, Dardia is focused on bringing personalized medicine programming to other Special Forces groups, veterans and units across the military.
At Thursday’s symposium, Dardia spoke on functional, performance medicine alongside health care professionals from the HunterSeven Foundation.

Members of SOCOM’s medical staff attended the three-hour conference in personal capacity, but SOCOM did not officially participate, according to a spokesperson.
“Our main focus is research and education, given that we are medical experts with advanced clinical licenses and degrees,” said Chelsea Poisson, an Army veteran, emergency nurse and clinical researcher with HunterSeven. “The attendees were extremely receptive, I had many questions from members across all communities on resources and what to do next.”
In addition to working with members of Congress to give suggestions and solutions to military health care legislature, HunterSeven provides TFDSOF with access to its extensive research on veterans health care issues.
“HunterSeven is working on legislation and research to get laws passed that provide our people with better access to health care quicker,” said Dardia. “They’re optimizing systems already in place, whether that’s in the DoD or at the VA.”
As functional, lifestyle-based medicine is adopted across the military, Dardia hopes to work himself out of a job. In years to come, the Green Beret hopes to begin correcting the problem of reactive health care in the civilian population, educating young people about disease prevention and holistic medicine.
“We want to advocate this not just for military personnel and veterans; this applies to everybody,” said Dardia. “This isn’t unique to the military. Cancer and suicide are rampant in the civilian population as well, and for the same reasons.”
Harm Venhuizen is an editorial intern at Military Times. He is studying political science and philosophy at Calvin University, where he's also in the Army ROTC program.




